Ripples of Despair - Shining a light on the impact of lives lost to alcohol, drugs, and suicide (2024)
Individual factors
The challenges individuals face are deeply shaped by their circumstances. Poverty, discrimination and abuse are just some of the structural issues that increase vulnerability. Life events like relationship breakdowns or homelessness can add to the risk of harm from alcohol, drugs and suicide. For those experiencing multiple disadvantages, these risks often overlap.
Children and young people: adversity, trauma and building resilience
The foundations for lifelong health and wellbeing are laid in early childhood. Positive experiences during this time are linked to better social and emotional development, stronger educational outcomes, and improved long-term health, including longer life expectancy (58,59). Conversely, adverse childhood experiences (ACEs), such as trauma, abuse, neglect or challenging environments, can lead to poorer outcomes like mental health challenges, unemployment, substance use, and homelessness (60,61).
The impact of adversity
While ACEs do not guarantee negative outcomes, they significantly increase the risk, particularly for children who face multiple adversities or live in poverty (62,63). Research shows that 85% of people in contact with criminal justice, substance use, and homelessness services experienced childhood trauma (64). Children who have been exposed to four or more ACEs as particularly vulnerable to poor health outcomes across the life course (65). However, many children overcome adversity when they have access to protective factors like stable relationships, supportive caregivers, and safe environments (60,63).
The pressures of child poverty, the cost-of-living crisis, and the lasting effects of the COVID-19 pandemic have increased these issues in the North, where child poverty rates exceed the national average (66).
For example, in Gateshead, the rate of alcohol-specific hospital admissions for under-18s is nearly double the England average, highlighting the urgency for action.
Care-experienced children and young people
Care-experienced individuals are those who have spent time in foster care or children's home, and they face significant health and social inequalities (67-69). The factors underpinning and exacerbating these inequalities are often rooted in trauma and adverse childhood experiences and linked closely with poverty, education, housing, and many other building blocks of health (70).
They are at higher risk of mental health challenges, substance use, and premature death, often from "unnatural causes" like suicide or drug-related deaths (67,68,71,72). Children in care, often due to the trauma of abuse or neglect, may experience greater levels of drug and alcohol harm compared to their peers and are over four times more likely to attempt suicide than their peers (73,74).
Building resilience
Resilience is the ability to adapt to stress and adversity, and it can protect children from long-term harm. Positive relationships with parents, caregivers, friends, teachers, and wider support networks are critical, as they provide the stability and support needed to develop coping skills and build self-esteem (64). Building resilience is not a quick fix. It requires sustained, long-term support and interventions (3). Resilience-building strategies include:
- Creating safe, trusting environments for children
- Providing opportunities to build self-esteem and a sense of control
- Strengthening family relationships and addressing household challenges
- Offering community-level support and services to address broader inequalities
Gateshead's Health and Wellbeing Strategy reflects this commitment, prioritising "giving every child the best start in life", with a focus on conception to age two as a critical period for intervention (75). The Early Help Strategy (2023-26) builds on this by expanding Family Hubs and programmes to support family stability and reduce risks before they become set in.
By addressing individual and community risk factors, Gateshead aims to create environments where all children can thrive, breaking cycles of adversity and promoting wellbeing for generations to come.
Case study - Trusting Hands Gateshead
Trusting Hands Gateshead (THG) is a multidisciplinary team of mental health practitioners, employed by the Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (CNTW), THG works with Gateshead Children's Social Care services to deliver trauma-informed care.
The service name, 'Trusting Hands Gateshead: Strengthening connections through stories, safety, compassion and care', was developed with input from young people in Gateshead residential care homes, supported by Gateshead Young Ambassadors.
THG aims to:
- Understand and address the emotional and mental health needs of vulnerable young people
- Support families and systems around young people to promote stability and resilience
- Enable young people with complex needs to thrive
Demographics
Age
Deaths due to alcohol, drugs and suicide are most common in middle age. Between 2019 and 2021, the highest mortality rates were among 45-60-year-olds (3). While middle-aged adults have the higher number of deaths, young adults face a disproportionate risk: alcohol, drugs and suicide accounted for 41% of all deaths among 25-29-year-olds (3).
Generation X, who are those born in the 1960s and 1970s have continued to have high rates of deaths from drug poisonings and suicide for the past 30 years (76). This may be linked to opioid use and the increasing health effects of ageing (76,77), alongside experiences of risks such as financial instability, and unemployment (76). This evidences highlights the need for action to protect future generations when facing adversity.
Ethnicity
Suicide and alcohol-specific deaths are most common in White and Mixed/Multiple ethnic groups, with Indian males also experiencing elevated alcohol-related death rates (78,79)
Alcohol-specific deaths age-standardised mortality rate per 100,000 in England and Wales 2017-2019 (79)
| Ethnicity | Males | Females |
|---|---|---|
| White | 15.3 | 8.1 |
| Mixed/Multiple Ethnic Groups | 12.5 | 8.2 |
| Indian | 16 | 1.9 |
| Bangladeshi | 0 | 0 |
| Pakistani | 2.5 | 0 |
| Asain Other | 7.5 | 1.5 |
| Black African | 2.5 | 2.2 |
| Black Caribbean | 3.3 | 2.4 |
| Black Other | 6 | 2.7 |
| Other ethnic group | 4.8 | 0.9 |
The National Programme on Substance Use Mortality data from 1997 to 2023-2024, indicates that where ethnicity is known and recorded at death registration, the majority of deaths involving illicit substances are among those of white ethnicity at 96.1% (80).
However, ethnicity data is often incomplete, and 30% of drug-related death records lack this information (80). Barriers to care and targeted support for ethnic minority groups remain a significant concern.
Sex
Across all three causes, most deaths are among males. In 2022, across England and Wales, males accounted for three-quarters of suicides, two-thirds of all drug poisonings, and two-thirds of alcohol-specific deaths (28,29).

Women between the ages of 16 and 24 are almost three times as likely (26%) to experience a common mental health issue as males of the same age (9%), and women are twice as likely to be diagnosed with anxiety as men (82,83). However, women are more likely to seek support (84).
Men in the UK have reported lower levels of life satisfaction, happiness, and the feeling that what they do in life is worthwhile, than women, according to the national wellbeing survey 2016-17 (85). Men are also less likely to seek help, often using substances as coping mechanisms for poor mental health, exacerbated by gender norms that discourage vulnerability (84) (86).
LGBTQ+ community
Lesbian, gay, bisexual, trans, queer, and questioning (LGBTQ+) people face significant health inequalities throughout their lives. (87) Discrimination (both within and outside of healthcare), unmet needs, barriers to accessing appropriate support and negative experiences when accessing support all contribute to worse health outcomes.
It is difficult to assess rates of deaths due to alcohol, drugs, and suicide for those who identify as LGBTQ+ in the UK as sexual orientation and gender identity are not recorded on death certificates. (88) However, research in this area suggests the LGBTQ+ population experience a higher risk of mental ill health, self-harm, and suicidal behaviour (88), in addition to higher levels of hazardous drinking and illicit drug use (89-91). Inequalities in access to healthcare exist for the LGBTQ+ population and these barriers to care impact people accessing the support they need (88,89).
Neurodivergence
Neurodiversity is a term used to describe the natural variations in the ways all our brains work (92-94). Neurodivergence includes Autism, Attention Deficit Hyperactivity Disorder (ADHD), Tourette's Syndrome, Dyslexia, among other conditions. Research indicates that autistic people are more at risk of suicidal ideation and attempted suicide than the general population, and the number of autistic people dying by suicide is approximately 2-8 times higher than those who are not autistic (95).
Potential underlying factors, specific to autism, which may increase suicide risk include masking or hiding autistic traits to fit in, which is detrimental to mental health, repetitive thoughts which can lead to rumination and feeling trapped; and lack of appropriate support (95). Autistic people have been identified as a priority group in the national suicide prevention strategy (96).
ADHD is also linked to an increased risk of suicidal ideation and substance use due to co-occurring mental health challenges like anxiety and depression (97-105).
Pregnancy
Perinatal mental health issues impact over 1 in 4 pregnant women and new mothers (106) and suicide is the leading cause of death during the period from 6 weeks to 1 year postpartum, with an increased risk for women facing multiple adversities (107,108).
For women experiencing drug and or alcohol issues, there is an intense stigma around pregnancy, birth and postnatal. It can be difficult to access the support they need to manage their mental health whilst caring for themselves and their children. Some mothers face the additional trauma of their children being removed (107). Pregnant or postnatal women who are experiencing adversity and disadvantage often experience feeling judged, misunderstood, shame and guilt. This can subsequently exacerbate their struggles with substances and contribute to further deterioration in their mental health (107).
Health status
Conditions such as chronic pain and respiratory illnesses like chronic obstructive pulmonary disease (COPD) are common among those with substance use issues (109,110). Chronic pain doubles suicide risk and can lead to substance use as a coping mechanism, further complicating care (109,111). For example, approximately 50% of alcohol and drug use disorder patients are affected by chronic pain (109).
Mental health and self-harm
Around 1 in 4 suicides in England are people who are known to mental health services(96).Mental health conditions such as borderline personality disorder, anorexia nervosa, depression, bipolar disorder, and schizophrenia increase suicide risk (112). Dual diagnosis is where substance use disorder and mental illness co-occur, this can present additional barriers to care, as services often focus on one issue rather than addressing both simultaneously (113,114).
Self-harm is "an intentional act of self-poisoning or self-injury, irrespective of the motivation or apparent purpose of the act and is an expression of emotional distress" (115) and is a major risk factor for suicide. In Gateshead, emergency hospital admissions for self-harm are significantly higher than the national average (14), particularly among young people aged 10-14 where it is double the rate in England (116), indicating a critical need for mental health support locally.
Socio-economic position
Poverty
Living in poverty impacts people, and their health, throughout their lives (58). It goes beyond a lack of money—it's the constant stress, scarcity of resources, and loss of control and dignity that take a toll on mental and physical health. Living with debt is particularly damaging, linked to adverse outcomes, including deaths due to alcohol, drugs, and suicide (58). This constant strain, known as economic adversity, forces people to focus on immediate survival, often leaving little capacity to plan for the future.
The graphs below show the link between deprivation and death by alcohol, drugs and suicide. The most deprived 10% of areas have markedly higher rates of deaths from alcohol, drugs, or suicide than the least deprived 10% of areas.
Alcohol-specific mortality in England in 2021(directly standardised rate per 100,000, County & UA deprivation deciles IMD 2019, 4/21 geography).
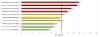
(117)
Those with lower socio-economic status suffer greater harm from alcohol, even though they tend to drink similar or lower amounts compared to wealthier groups - a phenomenon known as the "alcohol harm paradox". (118,119)
This highlights how other factors, such as access to healthcare and nutrition, may amplify the risks for populations experiencing deprivation.
Deaths from drug use in England in 2020-2022(Directly standardised rate - per 100,000, County & UA deprivation deciles, IMD 19, 4/23 geography)

(120)
For deaths by suicide, the County & UA deprivation deciles do not demonstrate the same trends, potentially due to lower numbers of deaths across large geographic areas masking inequalities. Suicide also occurs at higher levels in some rural areas, which are generally less deprived (52,121). However, there is a clear difference of rates by level of deprivation when looking at data for smaller local areas (LSOAs).
Suicide rate in England 2019-2021(persons 10+ years, directly standardised rate per 100,000, LSOA 11 deprivation deciles IMD 2019)

(22)
Insecure work, low wages, cost of living, inflation, insufficient benefit provision all contribute to an economic landscape where poverty and deprivation are unavoidable for many (58). Unfortunately, the reality is not as simple as finding a job and earning enough money to move out of poverty. We know that more people are working and remain in poverty (58,122).
Employment status
Unemployment is strongly linked to poor mental health and is a risk factor for harmful drinking, drug use, suicide, and homelessness (123-125). During times of economic recession, unemployment often leads to psychological distress, which increases substance use as a coping mechanism. During these times, providing psychological support for those who have lost their job and are vulnerable to drug use is essential (126).

The Dame Carol Black review highlighted employment is an essential part of recovery from substance use, for both financial stability and to offer something meaningful to do (127).
According to the World Health Organization, decent work can improve mental health, but also provides a sense of purpose, confidence, and routine. It builds social connections and supports recovery for those with mental health or substance use issues (128).
However, people with drug issues face significant barriers to employment, including stigma, receiving treatment whilst working, mental and physical health challenges, and lack of skills or training. Addressing these obstacles requires both individual support and broader societal changes (129). Rates of employment for people with severe mental illness are particularly lower than for any other group of health conditions, underscoring the need for tailored interventions (130).
Case study - Individual Placement Support (IPS)
Gateshead & South Tyneside's Individual Placement Support (IPS) initiative connects job seekers in recovery from addiction with meaningful employment opportunities. Embedded within local drug and alcohol services, IPS has helped over 100 individuals secure sustainable jobs.
Across the two local authorities, the team believes that everyone in our communities deserves a fair chance, so works hard to help people in recovery to find meaningful and sustained work. Employers are also a key part of supporting the initiative, and work with Gateshead & South Tyneside IPS to offer new roles and opportunities throughout the year.
Contextual factors
Stressful life events such as relationship breakdowns, chronic illness, or bereavement can increase susceptibility to substance use disorder and suicide. (131,132) Childhood maltreatment is also a significant risk factor for early substance use and long-term alcohol problems (131). While these factors do not guarantee harm, understanding them helps target resources and support where they are most needed.
Exposure to conflict, violence and war: asylum seekers and refugees
Inequalities experienced by refugee and asylum-seeking populations throughout their lives may contribute to factors increasing risk of harm by alcohol, drugs and suicide. While refugee and asylum-seeking communities are diverse groups, people that have been displaced are likely to have common experiences related to being on the move.
Factors during migration journeys may include issues such as poor living conditions and fears that come with being trafficked. They may feel a sense of shame, or guilt, at having to have fled their country of origin - perhaps leaving loved ones and their homeland behind. Their living standards may be drastically different from their home country, lacking basic services and often experiencing violence and detention (133).
Stigma may be felt by those with a refugee and migration background upon their arrival into their host country. This may be surrounding barriers to accessing healthcare and other services, poor living conditions, separation from support networks and family, uncertainty surrounding work permits and legal status, and in some cases, immigration detention (133). There are also challenges around adapting to change, potential unemployment, racism and exclusion, social isolation and possible deportation (133).
Poor mental health is common and may include symptoms of anxiety and depression, PTSD, suicidal ideation and/or attempts, along with substance use disorders (134). Substance use is often initiated or increased after experiencing trauma, to self-medicate and avoid difficult emotions (134). Women and unaccompanied minors are particularly vulnerable, facing risks such as exploitation and harassment, correlating with substance use (134).
Exposure to conflict, violence and war: veterans
Veterans experience higher rates of depression, Post Traumatic Stress Disorder (PTSD), and alcohol misuse compared to civilians (135,136). PTSD in particular can co-occur with problematic alcohol use (135,136).
Services like the Armed Forces Outreach Service and Walking with the Wounded report that alcohol misuse is a factor in up to 60% of referrals (137).
While suicide rates among veterans are generally lower than the general population, young early service leavers are at higher risk (137,138).
Domestic abuse
Domestic abuse has severe physical and mental health consequences for victims and survivors. Those experiencing domestic abuse are more likely to have substance use needs and experience homelessness (139). Rates of domestic abuse in the North East are higher than England, and drug-related deaths, suicide, and domestic homicides are more common in women experiencing abuse (139).
In 2021, women in the North East of England were 1.7 times more likely to die early because of suicide, addiction, or murder by a partner or family member than in the rest of England and Wales (140).
Rates of domestic abuse related incidents and crimes have been increasing, and Gateshead has higher levels than England, with 38 incidents per 1000 people in 2022/2023 (141). Among victims and survivors in Gateshead, data shows also increasing additional needs, with mental health needs most common (139).
Tragically, suicide is increasingly recognised as a consequence of domestic abuse, with 93 of the 242 domestic abuse-related deaths in England and Wales in 2022/23 being suicides (142).
There is therefore a strong association between substance use and domestic abuse - as a risk factor for perpetration and victimisation of domestic abuse. Perpetrators of domestic homicide have been found to have high rates of alcohol and/or drug use (143-146).
Homelessness
In 2022-2023, over 1,600 households in Gateshead faced homelessness(147).Homelessness severely impacts mental and physical health, with many people experiencing substance use, mental health challenges, and trauma (148,149). Children in these households are also affected, with impacts on their education, mental health, and family stability (123).
The health inequalities and poor health outcomes faced by those experiencing homelessness are stark. For those who are sleeping rough, there are significant needs related to mental health, drugs and alcohol (148,149).

The root causes of homelessness, including poverty, lack of affordable housing, and unemployment, are intertwined with the risk factors for alcohol, drugs, and suicide (149). Addressing these systemic issues is critical to reducing harm and promoting recovery.
Experience of the criminal justice system
People in contact with the criminal justice system face significantly higher risks of suicide and drug-related deaths. Offenders in the community are approximately six times more at risk of suicide than the general population, and the risk of drug-related death amongst this population is 16 times higher (150). Female offenders are at even greater risk, with rates of suicide and drug-related deaths 11 and 33 times higher respectively than the general population.
Barriers to accessing appropriate support further exacerbate these inequalities. Addressing health disparities in this population can improve overall wellbeing and reduce reoffending rates (151).
